SOAP Note AI
About SOAP Note AI
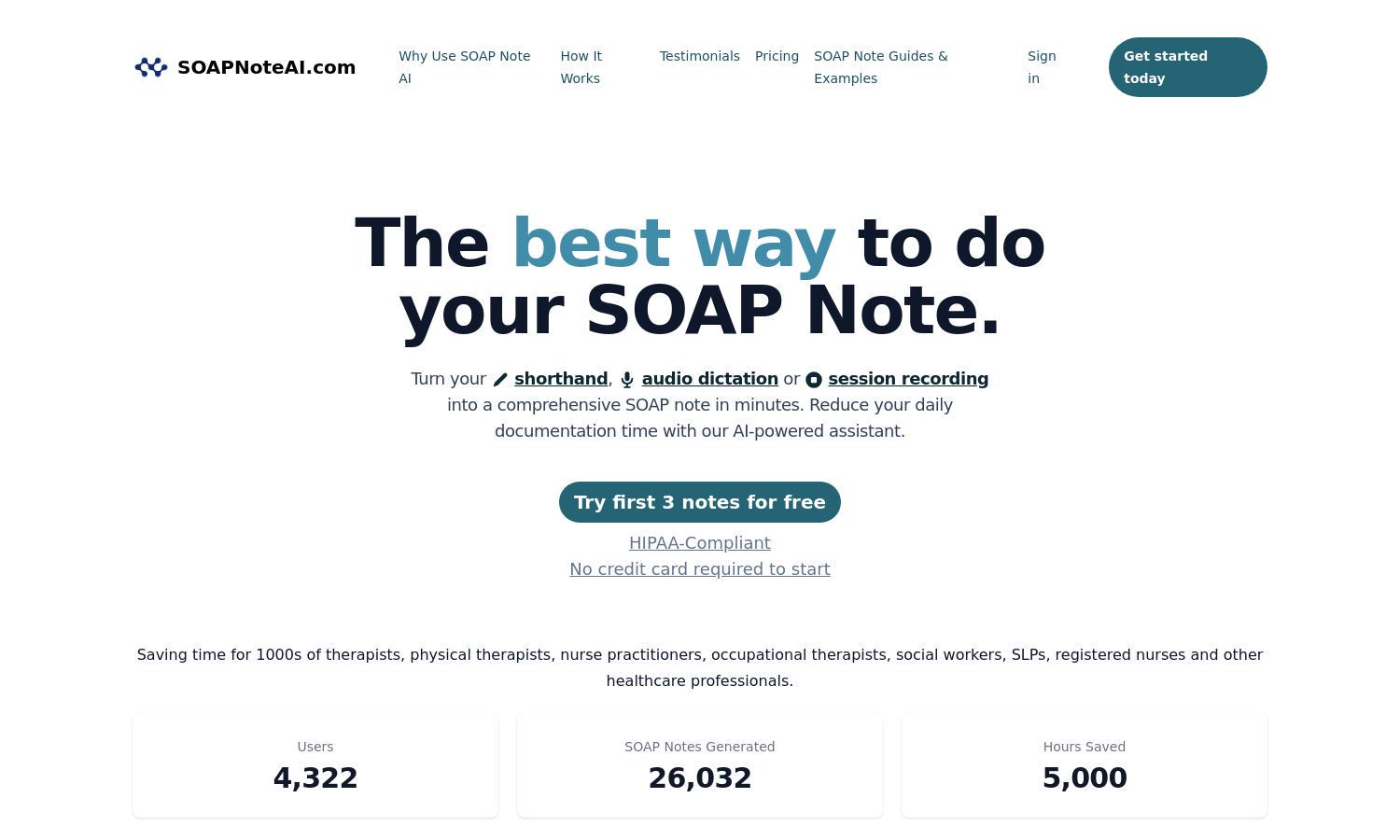
SOAP Note AI is designed for healthcare professionals seeking efficient documentation solutions. This HIPAA-compliant platform offers AI-powered generation of SOAP and Progress Notes across disciplines like physical therapy and mental health, significantly reducing documentation time and enhancing the accuracy of notes for better patient care.
SOAP Note AI offers flexible pricing plans starting with a free trial for up to 3 notes. Monthly subscriptions provide unlimited access for $69/month (Audio Only) or $79/month (All Notes). Pay-as-you-go options are also available, catering to diverse user needs while ensuring affordability and ease of use.
SOAP Note AI features an intuitive user interface that allows seamless navigation for generating SOAP notes. Its organized layout and interactive dashboard enable users to easily choose templates, input data, and review notes, making the documentation process efficient and user-friendly in professional settings.
How SOAP Note AI works
To use SOAP Note AI, professionals select their desired SOAP note template based on their field, then input information by typing, dictating, or recording. The platform auto-generates the Subjective, Objective, Assessment, and Plan sections. Users can review, edit, and download their notes, ensuring comprehensive documentation tailored to their needs.
Key Features for SOAP Note AI
AI-Powered Documentation
SOAP Note AI's AI-Powered Documentation feature minimizes time spent on note generation by automatically creating comprehensive SOAP notes from user inputs. This innovative functionality enhances workflow efficiency for healthcare professionals, allowing them to focus more on patient care rather than cumbersome documentation tasks.
Customized Templates
With SOAP Note AI's Customized Templates, healthcare professionals can choose from various template options tailored to their specific field. This key feature allows for greater flexibility in note-taking, improving documentation relevance and ensuring that all necessary information is captured accurately and efficiently.
Audio Dictation Support
SOAP Note AI includes Audio Dictation Support, enabling users to simply dictate their notes. This feature enhances usability for busy professionals by converting spoken words into structured SOAP notes, saving time and ensuring that important details are not overlooked during the documentation process.
You may also like: