Crosby Health
About Crosby Health
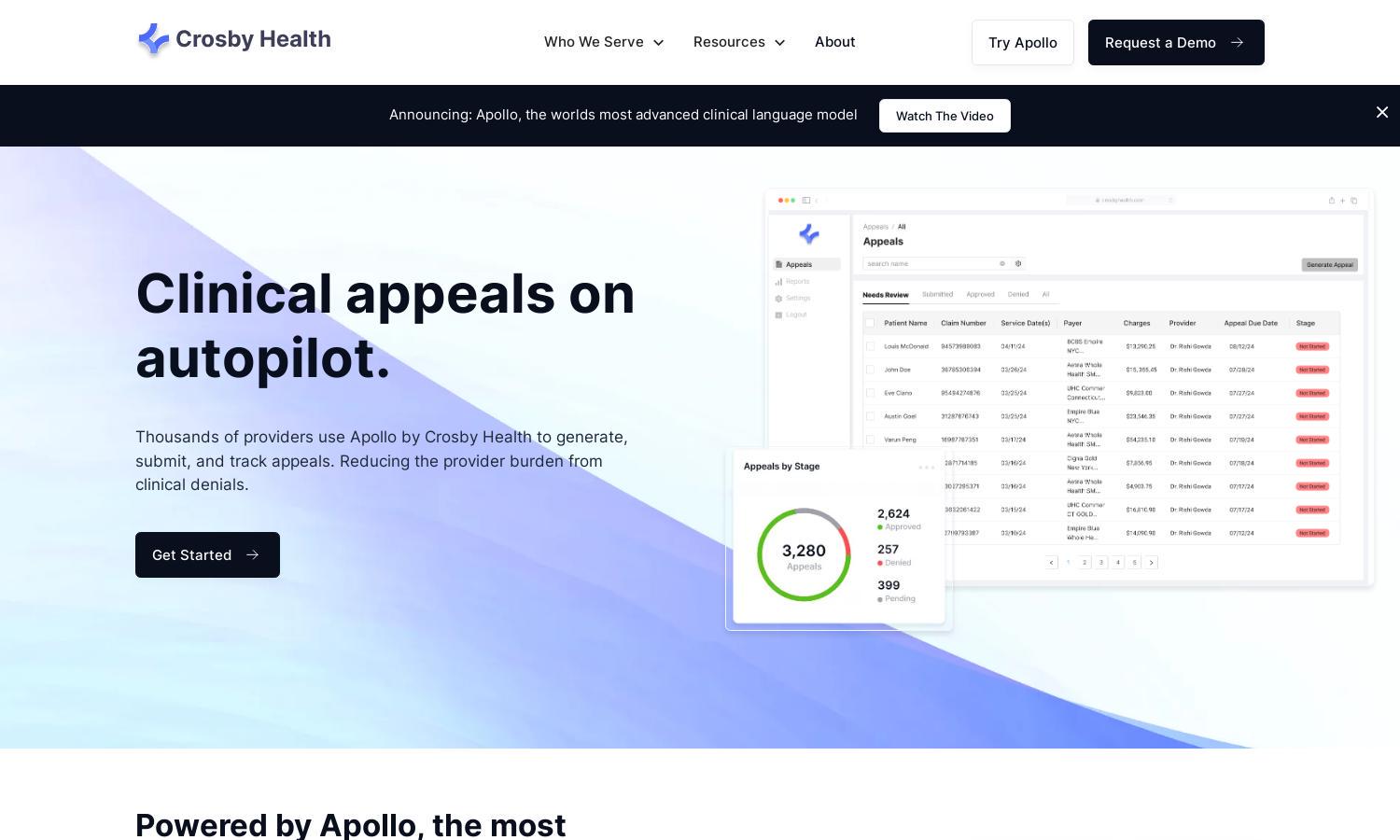
Crosby Health specializes in automated clinical appeals, serving hospitals, health systems, and private practices. Its innovative feature, Apollo, accelerates the appeal process by generating, submitting, and tracking appeals with clinical precision, empowering providers to overcome denials and focus on patient care effortlessly.
Crosby Health offers competitive pricing plans tailored to various provider needs. Each tier includes distinct benefits, such as enhanced access to Apollo's capabilities, offering users optimal value and efficiency. Upgrading unlocks additional features, improving appeal management and maximizing recovery potential.
Crosby Health features an intuitive user interface designed for seamless navigation. Its layout enhances the user experience, enabling easy access to all functionalities, including the sophisticated appeal generation tool. The clean design and actionable insights contribute to a productive workflow for healthcare providers.
How Crosby Health works
Users begin by onboarding with Crosby Health, where they integrate their existing systems. Once set up, navigating the user-friendly interface allows providers to generate appeal letters effortlessly. Apollo's AI crafts precise documents, submits them to relevant payors, and tracks their status, ensuring simplistic and effective denial management.
Key Features for Crosby Health
Automated Appeal Generation
Crosby Health's automated appeal generation feature leverages Apollo's advanced AI to streamline the creation of appeal letters. This unique capability reduces manual effort and enhances efficiency, allowing providers to respond swiftly to clinical denials while maximizing successful recoveries.
Unified Submission Platform
Crosby Health's unified submission platform simplifies the appeal process. Instead of managing multiple payor portals, users can submit all appeals through one interface, ensuring reliable tracking and instant notifications. This consolidated approach enhances workflow efficiency and minimizes administrative burdens for healthcare providers.
Real-Time Tracking Notifications
Crosby Health offers real-time tracking notifications, providing users with immediate updates on payor decisions regarding their appeal submissions. This feature allows healthcare providers to stay informed and responsive, significantly improving the management of clinical denials and ensuring timely follow-ups where needed.
You may also like:








